How to treat restless legs syndrome
Disclaimer: I am not a doctor and you should consult one before doing any of the below.
mini-tl;dr: RLS is linked to low iron levels in specific parts of the brain. Strongly consider having an iron infusion if your ferritin levels are <300 μg/l and transferrin saturation <45%. For many people this totally resolves their RLS in days to weeks, and will give at least some symptom relief for the majority.
You should ask for 1000mg ferric carboxymaltose or ferric derisomaltose as a total dose infusion.
tl;dr: Often physicians and even neurologists know little about treating RLS. Here is my (not a doctor) attempt at a treatment algorithm:
Do blood tests: full iron panel, vitamin D, B vitamins including folate.
Correct D + B vitamin deficiencies. Consider vitamin D megadoses. Consider removing any potential triggering medications (e.g. SSRIs, SNRIs, first-generation antihistamines), though fixing iron might negate the need for this.
Correct iron levels, preferably through IV iron infusion. Consider doing this even if your iron levels are normal, as long as ferritin levels <300 μg/l and transferrin saturation <45%.
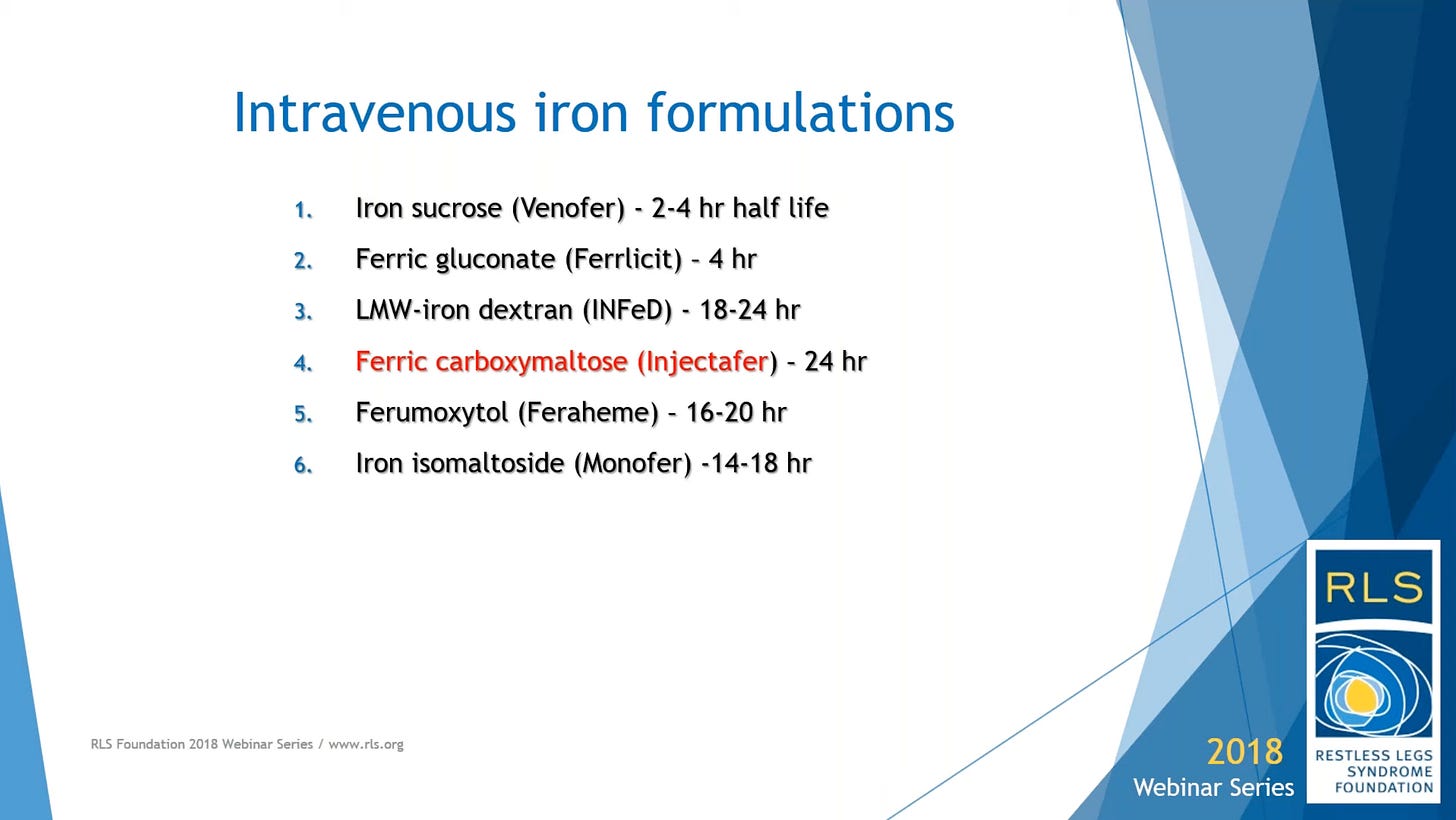
IV iron infusion: 1000mg of ferric carboxymaltose (Ferinject®) or ferric derisomaltose (Monofer®) as a total dose infusion. Full effect will be seen in 4–6 weeks. Retest iron levels after 8 weeks.
Oral iron also works and is cheaper, but can cause a lot of gastointestinal side effects and will often take many months. Brain iron deficiency is generally harder to correct than ‘body’ iron deficiency. Take 75mg ferrous bisglycinate (‘gentle iron’) + at least 100mg vitamin C, fasted, in the evening. Retest iron levels after 3 months.
Hopefully you’re done. If not, consider drug treatments (α2δ ligands, dopamine agonists, low-dose opioids).
Restless legs syndrome (RLS) is a pretty nasty condition. It’s pretty much impossible to really convey what it is to someone who hasn’t had it. Contrary to the name, it’s not really about moving your legs – it’s about unpleasant (unbearable) sensations in the legs, sometimes extending to the hands and feet and other parts of the body. Sufferers variously describe these as tingling, burning, tearing, like sparkling water is coursing through your veins. Moving the legs seems to relieve symptoms, partially and temporarily. Sometimes twitches occur as well, where your legs/hands/feet will jerk randomly.
It’s torture. The below is based on the research I’ve done into it after my symptoms started in mid-2022.
The full protocol
For someone who finds themselves suffering (relatively suddenly) with RLS, who isn’t pregnant or on dialysis (or has some other obvious explanation of why they might have RLS).
(Remember: I’m not a doctor. Nothing here is controversial; it's based on the latest best practice guidance from the International Restless Legs Syndrome Study Group task force1 with some other details added where useful.)
Have bloods taken: a full iron panel (to include iron, ferritin and transferrin saturation), B vitamins and vitamin D. Iron panel should be done fasted in the morning. If you’re taking iron supplements, stop taking them at least two days beforehand.
Correct any vitamin deficiencies you find. There’s some evidence that vitamins B1, B9 and B12 are involved in RLS, so take a B vitamin complex (I take Viridian High One, which has a high level of B1).
Your results will probably show your ferritin is low, perhaps even low enough to be classed as iron deficiency anaemia. If so, you need to replenish your iron stores.
If you have the money, have an iron infusion. This is indicated as first-line treatment for RLS as long as ferritin levels are <300 μg/l and transferrin saturation is <45%. Request 1000mg of ferric carboxymaltose (Ferinject®) or ferric derisomaltose (Monofer®) as a total dose infusion (i.e. don’t split it into multiple doses)2. In the UK this will probably cost at least £500 to have done privately, but if you’re anaemic you might be able to have one done on the NHS (might be worth saying you can’t tolerate oral iron for some reason). Unfortunately this doesn't work for everyone and takes up to 6 weeks for this to have an effect3; you should then have another iron test at 8 weeks.
Otherwise, supplement with oral iron following this protocol:
Ferrous bisglycinate (usually sold as ‘gentle iron’ in 14mg tablets), ~75mg + at least 100mg Vitamin C, taken once daily in the evening4 on an empty stomach.5 Re-test iron after 3 months.
Once ferritin levels are above 75, absorption slows. Consider taking a double dose every other night instead.6
Target ferritin levels are above 100 (from experience this will take many months), but there’s some evidence that RLS sufferers need to get it to 200 or 300 before they get relief.
You should also supplement vitamin D – it inhibits the production of hepcidin, a protein which blocks iron absorption. If your tests showed it was low (mine was), then consider high doses of vitamin D to correct that rapidly.
If you respond to IV iron but your symptoms start to come back some months later, you can have a repeat infusion as long as there has been a drop in your iron levels and you have ferritin <300.7
If this doesn’t work
If you’ve got your iron stores to high-normal and are still suffering, you might want to look at pharmacologic options. I know a lot less about the below; take with a pinch of salt.
First-line: α2δ ligands like gabapentin, gabapentin enacarbil, pregabalin. These are now preferred to dopamine agonists (which used to be the first-line treatment, and are miracle cures except that they end up making your RLS progressively worse).
Low-dose opioids like oxycodone, codeine, buprenorphine, methadone. Harder to get prescribed, but seem especially helpful for sufferers of severe RLS with painful features, and RLS patients seem not to develop tolerance to its effects in the same way as patients using opioids for pain relief.
Dopamine agonists like ropinirole, pramipexole, rotigotine. These used to be the first-line treatment for RLS but no longer. They have the risk of making your RLS considerably worse (presumably by upregulating expression of dopamine receptors, although I’m not certain) requiring dose increases; you risk eventually being on the maximum dose and then you’re stuffed. Withdrawing from these drugs is very unpleasant.
Why iron sometimes works
There’s a clear link between RLS and low levels of iron in the brain. This can be seen on MRI studies of people with RLS.
Iron stores are measured using ferritin (expressed in µg/L). Ferritin is a protein which binds to iron to regulate its release into the bloodstream. But for RLS, we don’t really care about iron in the bloodstream (unless you’re also anaemic) – we care about iron in the brain, which is pretty hard to measure.
Ferritin is a reasonable proxy for brain iron, but they’re not perfectly correlated. Thus, getting your ferritin to within the reference range might not be sufficient; some RLS sufferers need ferritin levels of 200 or 300 before getting relief. Your ferritin might not even be low in the first place. Presumably this is to do with dysfunctional brain iron homeostasis; why RLS sufferers experience this isn’t known. This video has a lot more information about this.
Note that ferritin is an acute phase protein; its level increases in response to infection, stress, and other insults, so your precise number can move around a lot and false high readings are possible.
This treatment algorithm is based on Allen RP et al. Evidence-based and consensus clinical practice guidelines for the iron treatment of restless legs syndrome/Willis-Ekbom disease in adults and children: an IRLSSG task force report. Sleep Med. 2018 Jan;41:27-44 [a] and Iron Biology: What We Should Know When Managing Restless Legs Syndrome, Earley 2018 [a], plus some helpful comments from the lovely people on the Health Unlocked forum.
Based on Earley 2018, who suggests that as the brain’s use of iron is greatest at night, it’s important to use an iron with a long half-life. Most studies in RLS have been done with ferric carboxymaltose. I was given ferric derisomaltose which has a similar, but slightly shorter, half-life. That all said, I suspect getting any iron infusion at all is better than nothing.
Earley 2018: “We wait for at least six weeks after because it appears to take six weeks for the brain to finally get enough iron and make the necessary alterations to improve the symptoms. Some patients may have improvements a few days after, maybe a week after, but if you’re going to have improvements it's likely to be seen and at its maximum at week six after the infusion.”
There’s evidence that brain the brain’s use of iron is circadian. Iron levels in cerebrospinal fluid are higher in the evening, suggesting this is when iron is taken up from the blood. This matters for individuals with RLS – “this has some implications on when one might want to consider taking iron. … If you’re trying to take iron so a large proportion gets into the brain, you might want to consider taking it at night.” from Earley 2018.
Some slides from that talk (it’s worth a watch):
Food reduces iron absorption, as does tea and coffee. For this reason I just found it easier to take in the evening a couple of hours after my last meal. It’s possible there are also good reasons for taking iron at night (see above footnote).
Taking oral iron causes the body to produce hepcidin; this blocks iron absorption. Allowing 24h+ between doses gives your body time to clear the hepcidin. See Stoffel NU et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020 May;105(5):1232-1239.
Earley 2018: “If the patient responds to the initial iron infusion as established at the 6 week … endpoint, then I will repeat the IV iron infusion if the patient’s RLS symptoms worsen and there is an associated drop in their iron levels – so long as their ferritin is less than 300.”